
These account for more than 75% of all tachyarrhythmias, both atrial and ventricular.
Atrial tachycardias can usually be rate controlled with beta-blockers or calcium channel blockers. APPROPRIATE sinus tachycardia (due to concurrent sepsis/anaemia/thyrotoxicosis/pain) should be left alone and the underlying trigger treated. INAPPROPRIATE sinus tachycardia can be slowed using beta-blockers or ivabradine (selective sinus node blocker), however it is usually best left alone. P waves are often hidden in the QRS complex. The impulse originates from the AV node and propagates to the atrium and the ventricles simultaneously. high vagal tone, sick sinus syndrome), the AV node takes over. If the sinoatrial node is not functioning (e.g. The atrioventricular node is the next most autonomic piece of tissue in the heart after the sino-atrial node. 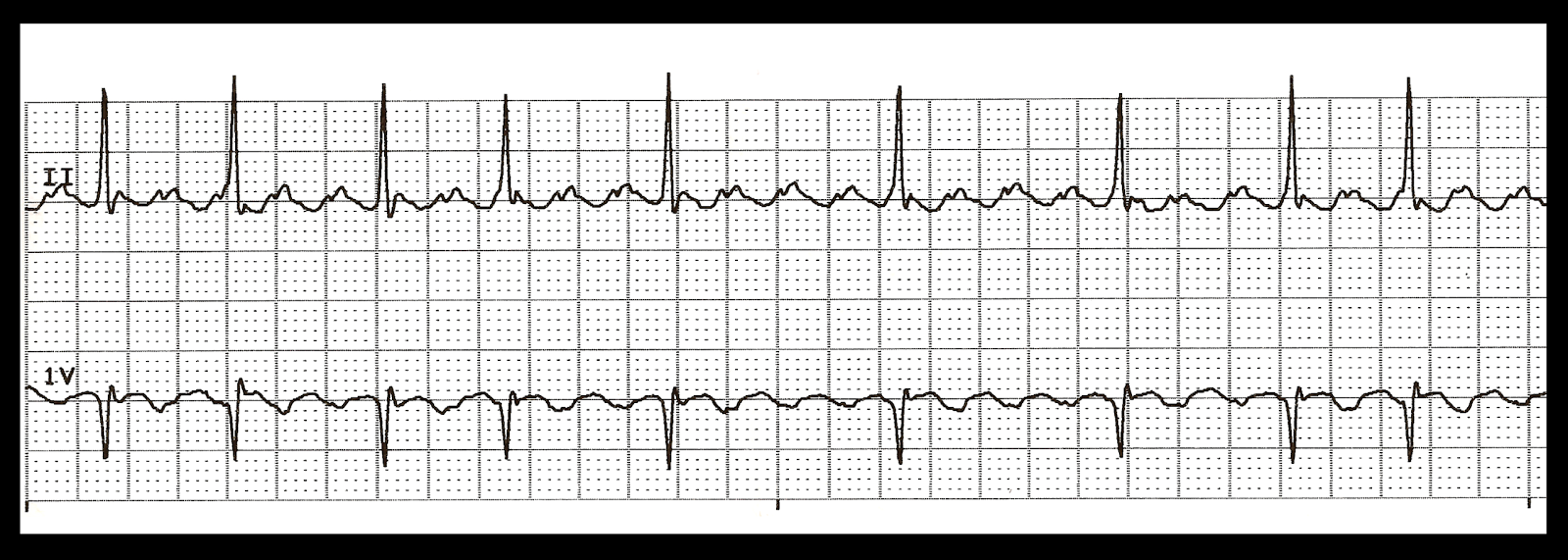 Similar to atrial tachycardia in all other respects. The P waves will have different morphologies as the atrial focus changes from beat to beat. COPD)Ītrial tachycardia Multifocal atrial tachycardia Atrial tachycardia is common amongst patients with concomitant lung disease (e.g. ‘Normal’ P waves should LOOK like a regular P wave and should be POSITIVE in the inferior leads (as they originate from the top of the atrium and propagate towards the inferior lead). Often seen in patients with chronic lung disease. A different focus in the atrium takes over from the sinoatrial node resulting in ABNORMAL P waves preceding QRS complexes. You might also be interested in our medical flashcard collection which contains over 2000 flashcards that cover key medical topics. This means there will be an organised atrial contraction and a wave similar to a P wave will appear before the QRS complex. If another part of the heart becomes MORE autonomic (or the sinus node becomes LESS autonomic), it takes over and a focal tachycardia results. Also knows as ‘enhanced automaticity’ – the sinus node is meant to be the most autonomic part of the heart and as such takes charge. The tachycardia originates from a single point (or points) in the atrium or AV node. To divide up this myriad of possibilities, a bit of basic electrophysiology terminology needs to be applied.
Similar to atrial tachycardia in all other respects. The P waves will have different morphologies as the atrial focus changes from beat to beat. COPD)Ītrial tachycardia Multifocal atrial tachycardia Atrial tachycardia is common amongst patients with concomitant lung disease (e.g. ‘Normal’ P waves should LOOK like a regular P wave and should be POSITIVE in the inferior leads (as they originate from the top of the atrium and propagate towards the inferior lead). Often seen in patients with chronic lung disease. A different focus in the atrium takes over from the sinoatrial node resulting in ABNORMAL P waves preceding QRS complexes. You might also be interested in our medical flashcard collection which contains over 2000 flashcards that cover key medical topics. This means there will be an organised atrial contraction and a wave similar to a P wave will appear before the QRS complex. If another part of the heart becomes MORE autonomic (or the sinus node becomes LESS autonomic), it takes over and a focal tachycardia results. Also knows as ‘enhanced automaticity’ – the sinus node is meant to be the most autonomic part of the heart and as such takes charge. The tachycardia originates from a single point (or points) in the atrium or AV node. To divide up this myriad of possibilities, a bit of basic electrophysiology terminology needs to be applied. 
It is a blanket term that includes a lot of different rhythms and is simply a starting point on the road to diagnosis. However, with a bit of thought (and possibly some adenosine), the underlying diagnosis can be revealed and appropriate treatment can be started.įirstly, a statement…SUPRAVENTRICULAR TACHYCARDIA IS NOT A DIAGNOSISĪ ‘supraventricular tachycardia’ is a rapid heart rate that originates from above or within the atrioventricular (AV) node. It describes any fast heart rate that you aren’t sure what it is and usually triggers an immediate cardiology referral after a certain amount of panic. ECG Blog #132 (Ventricular Tachycardia - VT - Vfib.Everyone loves the term ‘supraventricular tachycardia’.ECG Blog #133 - Is there AV Dissociation?.ECG Blog #134 - Is there AV Dissociation?.ECG Blog #135 (Regular WCT – Fascicular VT – RBBB.ECG Blog #136 - Run of Narrow, then Wide Beats.ECG Blog #137 (SVT – AV Block – Atrial Flutter – A.

ECG Blog #138 (SVT – AV Block – Atrial Flutter – A.ECG Blog #139 (Atrial Flutter – AV Block – Artifac.There is also an area of "overlap" between atypical forms of AFlutter and ATach - for which distinction lies in the realm of the EP cardiologist. NOTE - Practically speaking, distinction between ATach and AFlutter matters little in the acute setting - since initial treatment of these 2 entities is similar (ie, use of AV nodal rate-slowing medication).Of atrial activity is at least slightly below the usual range for flutter.

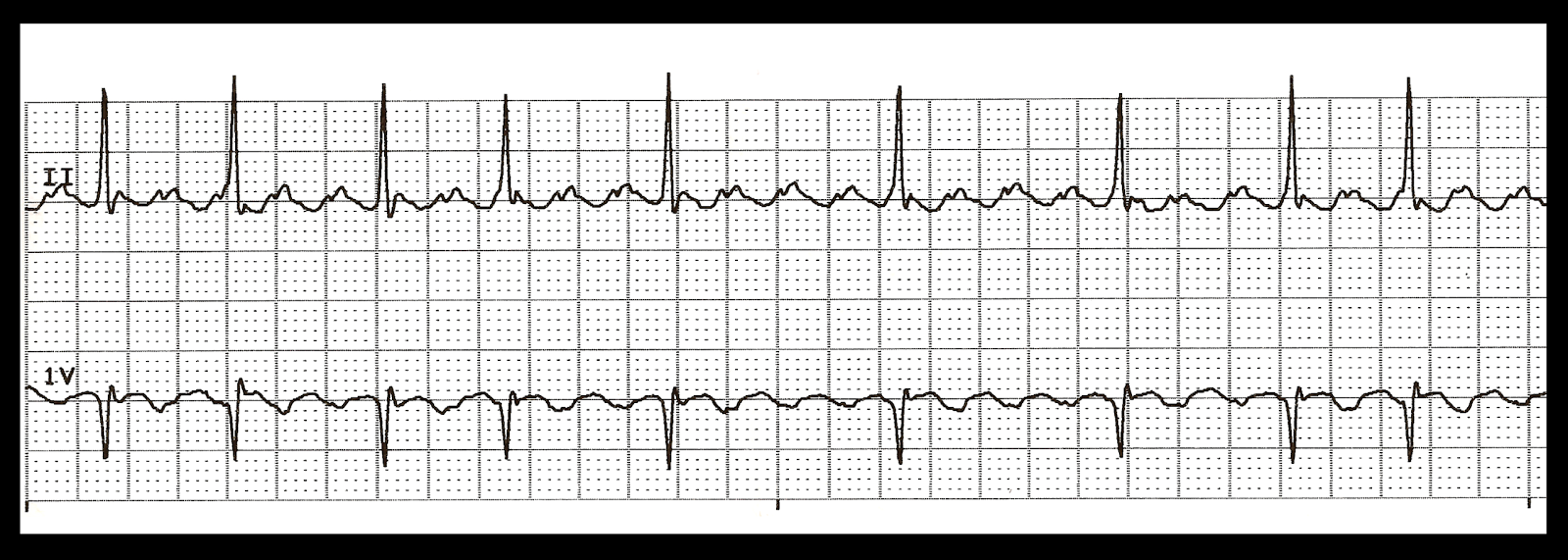
When the characteristic sawtooth appearance of flutter is missing, and the rate Tachycardia ) and AFlutter may be difficult. Subtle and only seen in a handful of leads ( if That said, flutter waves may sometimes be Typically manifests a sawtooth appearance that is usuallyīest seen in the inferior leads. Unless the patient is on antiarrhythmic medication or has WPW ( Wolff-Parkinson-White) Syndrome. Ratios (ie, 1:1: 3:1 5:1 ) are possible, but extremely uncommon Less commonly with atrial flutter - there is 4:1 AV conduction ( ventricular.







 0 kommentar(er)
0 kommentar(er)
